Background
About Opioid Substitution Treatment/Drug Related IssuesThe Tauranga Opioid Substitution Treatment service (OST) is one of the services offered by Bay of Plenty Addiction Service (BOPAS) that is part of Mental Health and Addiction Services, Bay of Plenty District Health Board (BOPDHB).
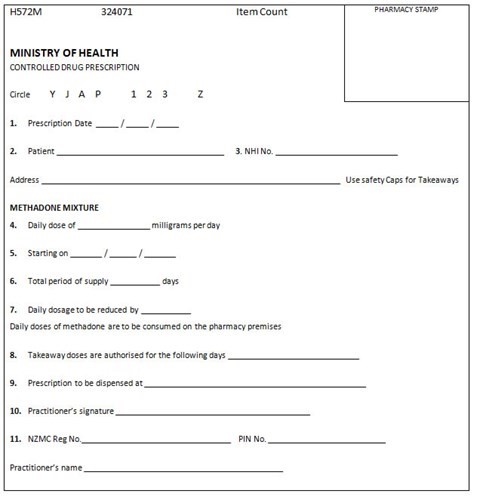
This pathway contains information and guidelines for General Practitioners authorized by BOPAS OST to prescribe methadone or buprenorphine/naloxone to patients in the GP Shared Care Programme. BOPAS OST intends that this information will assist in the provision of a quality, safe, professionally delivered OST Service that meets the needs of patients, their family/whanau, and the wider community. GPs and their staff are encouraged to consult with the Addiction Liaison Clinician or the Lead Clinician at BOPAS OST working in a shared-care partnership model.
BOPAS OST provides services for the management of opioid dependency from a harm reduction philosophy, supporting people towards recovery, relative to each individual and his or her own circumstances.
The OST programme is in accordance with:
The BOPAS Service manages the admission, stabilisation, and specialist maintenance phases of OST treatment. Patients may then be assessed as meeting criteria for the GP Shared Care Programme where their OST is integrated with their primary health care provider who is authorised by BOPAS on a three-monthly (6-monthly with permission from the MOH) basis to prescribe methadone or buprenorphine/naloxone.